While the foundational importance of nutrition is typically acknowledged by physicians and the media, nutrition is still not the focus of most medical care. Considering that estimates suggest around 60% of Americans have a chronic disease related to poor nutrition, this seems like a serious oversight.
And while nutrition is more commonly recommended for the prevention and treatment of diabetes, heart disease and physical health, it also plays a significant role in mental health. Using nutrition to improve mental health – such as supplementation, vitamin and mineral repletion, gut and digestive adjustments, and dietary changes – is often referred to nutritional psychiatry.
What is Nutritional Psychiatry?
Nutritional psychiatry explores the impact of diet and nutrition on mental health. It encompasses a wide range of evidence-based research, including the effects of individual nutrients, dietary patterns, the microbiome and gut health on a patient’s mental and emotional state.
The primary goal of nutritional psychiatry is to incorporate research-backed dietary and nutritional interventions to restore mental health as a first step in a patient’s recovery. Standard medications are usually only added once the nutritional impact of initial interventions is clear, and only when necessary.
Vitamins for Brain Function
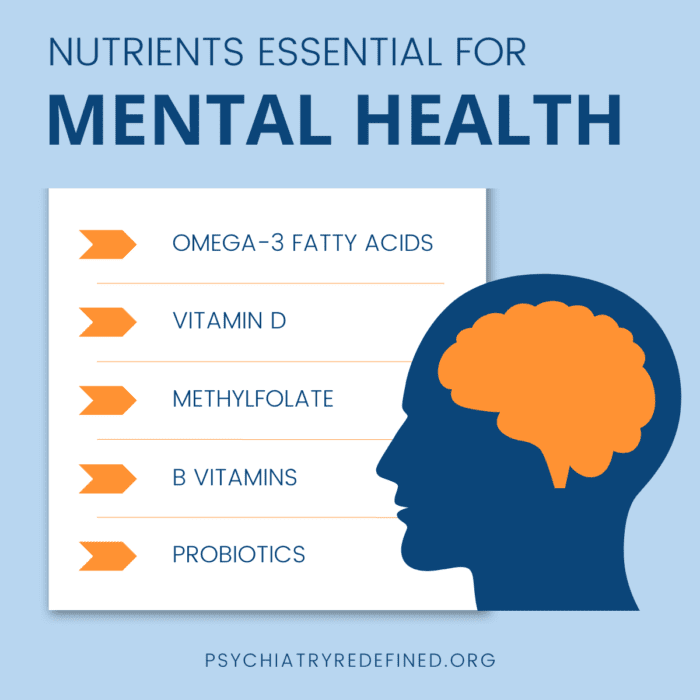
Numerous studies support the connection between diet, nutrition and mental function. Research continues to suggest benefits with the use of omega-3 fatty acids, probiotics, vitamin D, methylfolate and B vitamins, and minerals—including magnesium, zinc, copper and iron—among other nutrients, for supporting the brain, reversing mental illness, and influencing mood and cognition (Marx 2017).
Moreover, the gut-brain axis, a complex communication system between the gastrointestinal tract and the central nervous system, has become a focal point in nutritional psychiatry research (Mayer 2022). The gut microbiome, consisting of trillions of bacteria and other microorganisms, can produce neurotransmitters and influence immune function, including levels of inflammation. These influences can contribute both positively and negatively to an individual’s stress response and overall mental outlook.
Nutrition for Mental Health
As a practicing psychiatrist with decades of experience, my own patients have shown me how powerfully nutrition influences the brain. And it makes sense, since every component of our brain and body is derived from the food we consume. If a needed nutrient is in short supply, problems ensue.
As the founder of Psychiatry Redefined, evaluating a patient’s nutrient levels and treating deficiencies appropriately has been a foundational component of what we teach.
Nutrition is not an alternative, but a core component of whole-person health care.
Nutrition is fundamental to physical and mental medicine. If you want to stop managing your patients’ mental health symptoms and start treating the root causes of their mental illness, we encourage you to check out our growing community of mental health providers in our well-known Fellowship in Functional & Integrative Psychiatry. You’ll join thousands of other health care professionals making a huge difference in patient lives with nutritional medicine.
Ready to apply the latest nutritional therapies to combat mental illness with your patients? Enroll now in our Fellowship in Functional & Integrative Psychiatry!
References
Marx W, Moseley G, Berk M, Jacka F. Nutritional psychiatry: the present state of the evidence. Proc Nutr Soc. 2017;76(4):427-436. doi:10.1017/S0029665117002026
Mayer EA, Nance K, Chen S. The Gut-Brain Axis. Annu Rev Med. 2022;73:439-453. doi:10.1146/annurev-med-042320-014032


