Fewer and fewer doctors are choosing to specialize in psychiatry these days. One obvious reason is the poor efficacy of standard treatments. We become health-care providers to help people. However, patient recovery rates are discouraging, especially when relying solely on a poly-pharmacy approach to mental illness.
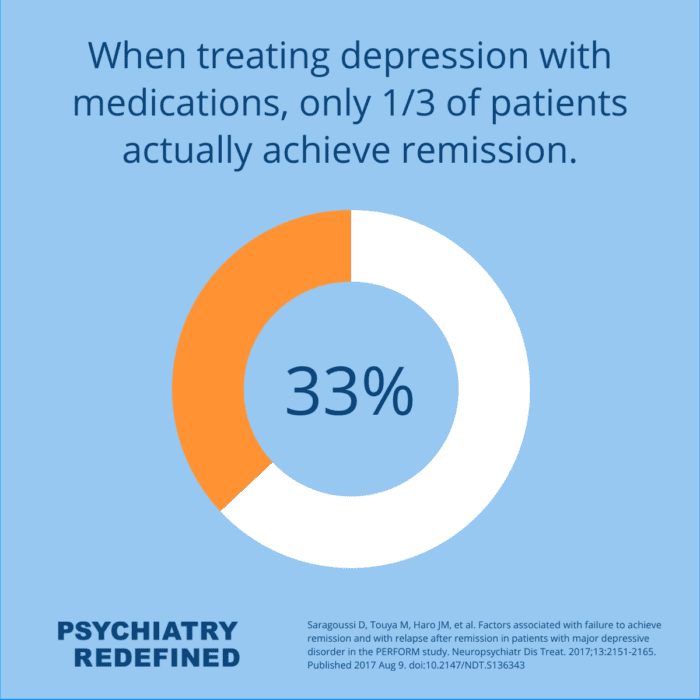
Consider this statistic: when treating depression with medications, only about one-third of patients actually achieve remission (Saragoussi 2017).
The practice of mental health care often becomes a process of juggling multiple medications, side effects and residual symptoms. Both the provider and patient are left unsatisfied, and symptoms persist.
Why Practice Functional Medicine?
This pharmaceutical approach to mental health can largely be attributed to the “Prozac Revolution” – a time in which the practice of psychiatry went through dramatic changes in marketing, prescribing and patient management. While this approach helped to sell medications, it curtailed much needed research, and destroyed attempts to personalize treatment. Pharmaceuticals became the “one-size-fits-all” treatment for all patients. Instead of addressing the underlying causes of mental illness, psychiatry opted to look the other way.
The inadequacies of the mainstream approach ultimately inspired me to pursue a more comprehensive clinical paradigm, one that not only acknowledged the role of biology in mental illness but placed it on equal footing with genetics, nutrition, trauma, lifestyle, and spirituality. This search led me to Functional Psychiatry — an integrated systems approach to mental health.
Functional Medicine for Mental Health
There is a better way – and that begins with personalized, whole-patient care.
For many years, research has shown that mental health is often influenced by physical health parameters. Nutrition, gut health, the microbiome, chronic infections, inflammation, hormone levels, genetics, toxicity and personal history all play a role in a person’s mental wellness.
Overlooking or ignoring ANY of these factors can lead to poor outcomes. It’s time we enhance psychiatric treatment with approaches that address whole-person wellness.
While medications can adjust neurotransmitters, this is only a small part of what influences our mood, cognition and mental health. With a comprehensive functional approach to mental health treatment symptom reduction is possible and mental wellness becomes attainable.
Rediscover Your Passion for Mental Health Care
Psychiatric care is in need of an upgrade. Poor patient outcomes and symptom management shouldn’t be the norm in mental health care. The career you imagined – helping people feel happier and mentally well – is possible with functional psychiatry.
With functional and integrative psychiatry education, like that provided through Psychiatry Redefined, thousands of mental health providers are changing patient lives across the globe. They are rediscovering their passion for helping patients. When patient outcomes are positive and lasting, practicing psychiatry can be fulfilling once again.
Psychiatry Redefined is one the leading resources for comprehensive, evidence-based continuing education. If you’re ready to rediscover your passion for patient care, we encourage you to join our supportive community and take the next step to elevate your career with the Fellowship in Functional & Integrative Psychiatry. You’ll discover the functional protocols your patients are seeking – and the skills to help you create the career you’ve always imagined.
Ready to learn how functional medicine can help your patients? Join our tribe and enroll now in our Fellowship in Functional & Integrative Psychiatry!
References
Saragoussi D, Touya M, Haro JM, et al. Factors associated with failure to achieve remission and with relapse after remission in patients with major depressive disorder in the PERFORM study. Neuropsychiatr Dis Treat. 2017;13:2151-2165. Published 2017 Aug 9. doi:10.2147/NDT.S136343