New research continues to reveal a powerful link between chronic inflammation and mental health problems. A recent meta-analysis linked depression, anxiety and post-traumatic stress disorder with higher levels of inflammation (Kuring 2023). In the study, the type of inflammatory response varied based on the diagnosis, yet all three diagnoses still showed significant associations.
Other conditions have also been shown to have correlations with inflammation, including bipolar disorder and schizophrenia (Solmi 2021, Zhou 2021). Identifying and treating any and all factors causing or contributing to the inflammatory response can be incredibly helpful for decreasing a patient’s symptoms.
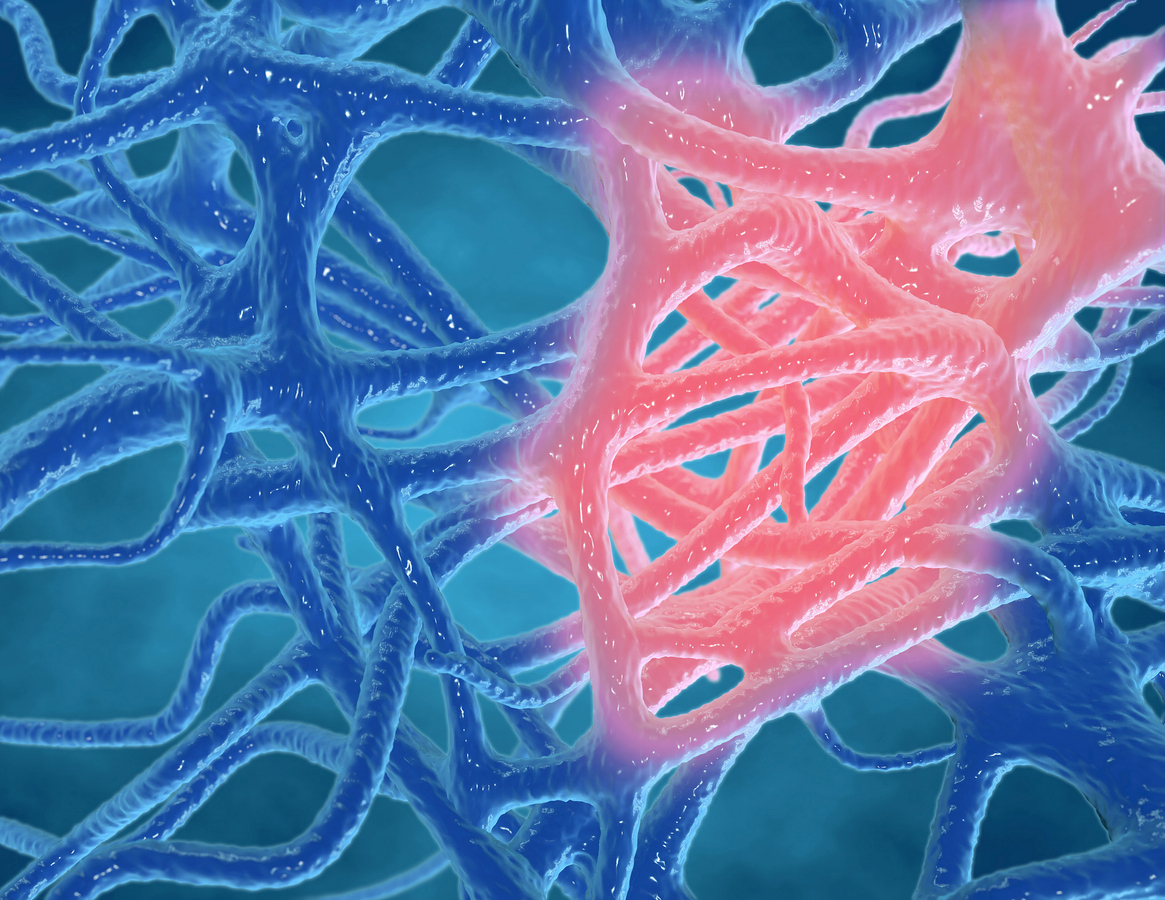
Inflammation and the Brain
When inflammation is present, it can cause problems through a number of different mechanisms, including damage to the blood brain barrier, increased glutamate levels and reductions in brain-cell growth factors.
The Blood-Brain Barrier and Inflammation
It shouldn’t be too surprising that inflammation, especially when chronic, can disrupt normal brain function. The brain is typically isolated from the rest of the body by the blood-brain barrier. Yet when chronic inflammation occurs, this barrier can become leaky, allowing more inflammatory molecules to make their way into the brain, further increasing inflammation and disrupting normal brain function (Futtrup 2020).
Glutamate and Brain Inflammation
In addition, inflammation in the brain can lead to toxic increases of glutamate (Haroon 2016). Glutamate is a neurotransmitter that revs up brain activity. When glutamate is present in excess quantities, it can over-stimulate brain cells causing their death in a process known as “excitotoxicity.”
Growth Factors and Brain Inflammation
And that’s not all of the problems caused by inflammation. When present, it can also disrupt brain cell formation, differentiation and growth, a process referred to as neurogenesis. One of the key promoters of neurogenesis is brain-derived neurotrophic factor (BDNF). Healthy levels of BDNF are crucial for healthy brain function. Yet when inflammation is present, BDNF production can become compromised, disrupting this key growth factor (Zhang 2016).
What Contributes to Chronic Inflammation?
When treating inflammation, it’s imperative that you know the underlying reason for the inflammation. Treating inflammation without knowing the cause is like throwing darts while blindfolded and hoping to hit a bullseye. It’s not an effective strategy.
Chronic inflammation can be attributed to numerous different factors that all can play a part in mental illness:
- Poor diet
- Nutrient deficiencies
- High stress levels
- Insufficient sleep
- Chronic infections
- Dysbiosis
- Food sensitivities or allergies
- Toxicity
All of these factors should be considered in any individual struggling with a mental health diagnosis. Once the causes are identified, treatment can directly target and resolve the inflammation by addressing the cause.
Directly Reducing Inflammation as a Treatment for Mental Illness
So the next obvious question becomes: does reducing brain inflammation improve mental health? The research appears to provide an emphatic yes!
Fish Oil
Omega-3 fatty acids from fish oil are well known for their anti-inflammatory effects. And the latest meta-analysis appears to confirm their benefits for treating depression. Fish oil supplementation was shown to have a significant effect for reducing depressive symptoms (Kelaiditis 2023). Testing for omega-3 fatty acid deficiencies can identify those individuals in need of omega-3 supplementation.
Curcumin
One of the most well-recognized natural anti-inflammatory agents comes from the kitchen spice turmeric. The color of turmeric is due to the presence of a yellow-orange polyphenol called curcumin. Curcumin supplements have been utilized in clinical trials for treating numerous inflammatory conditions, including anxiety and depression.
And results suggest that curcumin may be helpful. A meta-analysis of 10 trials found that curcumin provided large benefits for both depression and anxiety symptoms (Fusar-Poli 2020). Although promising, the researchers expressed caution in interpreting the results due to the small sample sizes.
As a treatment, curcumin can reduce elevated levels of C-reactive protein, a marker of inflammation that can be readily tested (Gorabi 2022). In patients with chronic inflammation from autoimmune diseases or other chronic causes, curcumin can be an effective tool.
Pine Bark and Grape Seed Extract: OPCs
Oligomeric proanthocyanidins (OPCs) are compounds that are found in high quantities in pine bark and grape seed extracts among other sources. They have also been shown to have strong antioxidant and anti-inflammatory effects (Ma 2020). Preliminary evidence has started to suggest benefits for mental health.
Proanthocyanidin intake has been shown to correlate with lower risks for depression (Chang 2016). In women with menopausal symptoms, pine bark extract had significant benefits over placebo for depression-type symptoms, including fatigue and feeling worthless. Improvements in anxiety were also showing trends for significance over placebo with reductions of 36% (Kohama 2013). Studies have also found significant effects comparable to standard medication with pine bark extract for treating the symptoms of attention-deficit/hyperactivity disorder (Weyns 2022).
Takeaway
Mental health is influenced by numerous factors, including inflammation. Identifying the cause and addressing chronic inflammation in patients struggling with mental health conditions can be a powerful strategy to help control symptoms and achieve remission.
Ready to learn more about treating inflammation in your patients?
Enroll now in our Fellowship! Book a private call with our faculty to learn more.
References
Chang SC, Cassidy A, Willett WC, Rimm EB, O’Reilly EJ, Okereke OI. Dietary flavonoid intake and risk of incident depression in midlife and older women. Am J Clin Nutr. 2016;104(3):704-714. doi:10.3945/ajcn.115.124545
Fusar-Poli L, Vozza L, Gabbiadini A, et al. Curcumin for depression: a meta-analysis. Crit Rev Food Sci Nutr. 2020;60(15):2643-2653. doi:10.1080/10408398.2019.1653260
Futtrup J, Margolinsky R, Benros ME, et al. Blood-brain barrier pathology in patients with severe mental disorders: a systematic review and meta-analysis of biomarkers in case-control studies. Brain Behav Immun Health. 2020;6:100102. Published 2020 Jun 30. doi:10.1016/j.bbih.2020.100102
Gorabi AM, Abbasifard M, Imani D, et al. Effect of curcumin on C-reactive protein as a biomarker of systemic inflammation: An updated meta-analysis of randomized controlled trials. Phytother Res. 2022;36(1):85-97. doi:10.1002/ptr.7284
Haroon E, Miller AH. Inflammation Effects on Brain Glutamate in Depression: Mechanistic Considerations and Treatment Implications. In: Dantzer R, Capuron L. (eds) Inflammation-Associated Depression: Evidence, Mechanisms and Implications. Current Topics in Behavioral Neurosciences, vol 31. Springer, Cham. 2016:173-198. https://doi.org/10.1007/7854_2016_40
Kelaiditis CF, Gibson EL, Dyall SC. Effects of long-chain omega-3 polyunsaturated fatty acids on reducing anxiety and/or depression in adults; A systematic review and meta-analysis of randomised controlled trials. Prostaglandins Leukot Essent Fatty Acids. 2023;192:102572. doi:10.1016/j.plefa.2023.102572
Kohama T, Negami M. Effect of low-dose French maritime pine bark extract on climacteric syndrome in 170 perimenopausal women: a randomized, double-blind, placebo-controlled trial. J Reprod Med. 2013;58(1-2):39-46.
Kuring JK, Mathias JL, Ward L, Tachas G. Inflammatory markers in persons with clinically-significant depression, anxiety or PTSD: A systematic review and meta-analysis. J Psychiatr Res. 2023;168:279-292. doi:10.1016/j.jpsychires.2023.10.009
Ma X, Wang R, Yu S, Lu G, Yu Y, Jiang C. Anti-Inflammatory Activity of Oligomeric Proanthocyanidins Via Inhibition of NF-κB and MAPK in LPS-Stimulated MAC-T Cells. J Microbiol Biotechnol. 2020;30(10):1458-1466. doi:10.4014/jmb.2006.06030
Solmi M, Suresh Sharma M, Osimo EF, et al. Peripheral levels of C-reactive protein, tumor necrosis factor-α, interleukin-6, and interleukin-1β across the mood spectrum in bipolar disorder: A meta-analysis of mean differences and variability. Brain Behav Immun. 2021;97:193-203. doi:10.1016/j.bbi.2021.07.014
Weyns AS, Verlaet AAJ, Breynaert A, Naessens T, Fransen E, Verhelst H, West DV, Van Ingelghem I, Jonckheere AI, Beysen D, Kenis S, Moens E, van Roest APJ, Savelkoul HFJ, De Bruyne T, Pieters L, Ceulemans B, Hermans N. Clinical Investigation of French Maritime Pine Bark Extract on Attention-Deficit Hyperactivity Disorder as compared to Methylphenidate and Placebo: Part 1: Efficacy in a Randomised Trial. J Funct Foods. 2022(97):105246. doi:10.1016/j.jff.2022.105246.
Zhang JC, Yao W, Hashimoto K. Brain-derived Neurotrophic Factor (BDNF)-TrkB Signaling in Inflammation-related Depression and Potential Therapeutic Targets. Curr Neuropharmacol. 2016;14(7):721-731. doi:10.2174/1570159×14666160119094646
Zhou X, Tian B, Han HB. Serum interleukin-6 in schizophrenia: A system review and meta-analysis. Cytokine. 2021;141:155441. doi:10.1016/j.cyto.2021.155441